Psoriatic Arthritis
Psoriatic Arthritis


Back to top
What is Psoriatic Arthritis?
Psoriatic arthritis (PsA) is a type of arthritis that causes joint pain, swelling, and stiffness in some people who have psoriasis. Psoriasis is a skin condition that causes flakey patches of skin which form scales. About 30% of people with psoriasis also develop PsA1,2,3.

PsA affects men and women equally. Prevalence of PsA ranges from 0.1% to 1% in the general population around the world4,5.
Back to top
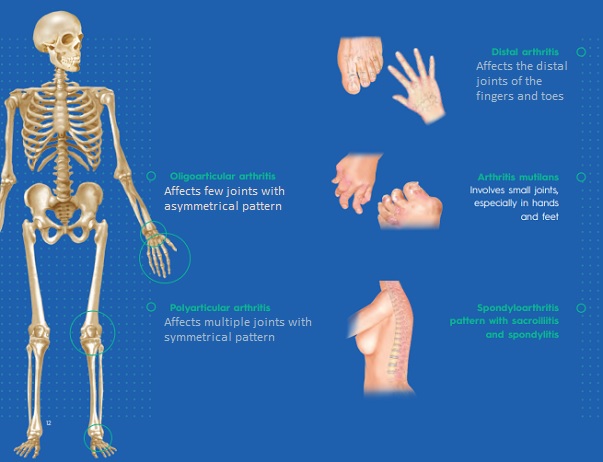
TYPES OF PSORIATIC ARTHRITIS
The clinical presentation of PsA is varied. The earliest classification of PsA by Moll and Wright included five subtypes:
Back to top
WHAT CAUSES PSORIATIC ARTHRITIS?
Researchers do not yet fully understand the causes of PsA. However, they believe that the disease develops due to a combination of genetic, immunologic, and environmental factors4,7. Genetic factors People with a family history of psoriasis or PsA are more likely to develop the conditions than those without5. More than 40% of people with psoriasis or PsA have family members with psoriasis or PsA7. Immunologic factors Both psoriasis and PsA are immunologically mediated and are autoimmune diseases, which means the immune system mistakenly attacks healthy tissue4,7. Environmental triggers Certain infections (human immunodeficiency virus, streptococcal infection) may also contribute to the development of PsA5,7. Mechanical/emotional stress or a physical trauma in genetically predisposed individuals have been identified as risk factors for developing PsA too5,6. People between the ages of 30–50 years are most likely to develop PsA. However, it may occur at any age3
Back to top
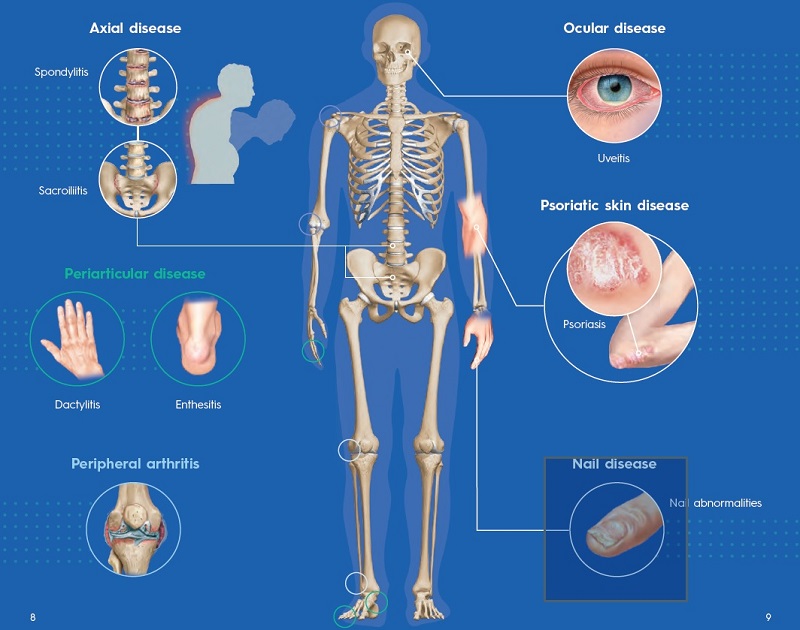
WHAT ARE THE ARTICULAR AND EXTRA-ARTICULAR MANIFESTATIONS OF PSA?
Patients with PsA present with pain and stiffness in the affected joints. Fatigue is also common3. The clinical features of PsA are described in terms of articular and extra-articular manifestations6:
Back to top
HOW WILL MY DOCTOR DIAGNOSE MY DISEASE?
Doctors diagnose PsA by obtaining the medical history, performing a physical examination, and taking x-rays of the joints to check for inflammation and joint damage. Blood tests or joint fluid tests may be done to rule out other diseases, such as rheumatoid arthritis and gout4 .
Back to top
WHAT ARE THE TREATMENT OPTIONS?
Treatment of PsA aims at relieving the symptoms such as joint inflammation and pain and slowing progression of the disease. The main medicines used to treat PsA are non steroidal anti-inflammatory drugs (NSAIDs), disease-modifiying antirheumatic drugs (DMARDs), and biologics1,4,7. NSAIDs NSAIDs are generally useful for symptoms of mild PsA6. DMARDs Conventional synthetic DMARDs such as methotrexate, or occasionally sulfasalazine, are useful to treat mild to moderate PsA6. Biologics Biologics function by inhibiting particular chemicals in the blood from activating the immune system attack on the lining of joints in the body. Severe peripheral arthritis usually receives treatment with biologics, especially tumor necrosis factor (TNF) inhibitors, which are particularly effective in PsA1,6.
Back to top
WHAT CAN I DO TO MANAGE MY DISEASE?
Non-pharmacological therapies, including physical therapy, occupational therapy, exercise program, and smoking cessation, should be strongly encouraged and incorporated in the treatment plan6 Pain and mobility
- Hot and cold therapies Heat reduces joint stiffness and muscle spasms. Cold decreases swelling4
- Physical and occupational therapy Physical and occupational therapists will establish a therapeutic home program and educate you about the disease and its management10
- Lifestyle Weight control Can improve response to medical treatments for PsA11 Exercise Strengthening and fl xibility exercises can help ease pain4
- Smoking and alcohol cessation Smoking and drinking too much alcohol can affect how medications for PsA work
Prognosis of PsA varies from mild joint disease to severe and deforming joint damage. Early treatment of PsA is associated with improved patient-reported outcomes8,9

Medical References
- NHS. Psoriatic arthritis. https://www.nhs.uk/conditions/psoriatic-arthritis/ (2019).
- NHS. Psoriasis. Overview. https://www.nhs.uk/conditions/psoriasis/ (2022).
- National Psoriasis Foundation. About psoriatic arthritis.https://www.psoriasis.org/about-psoriatic-arthritis/ (2021).
- Arthritis Foundation. Psoriatic Arthritis. https://www.arthritis.org/diseases/psoriatic-arthritis
- Karmacharya, P., Chakradhar, R. & Ogdie, A. The epidemiology of psoriatic arthritis: A literature review. Best practice & research. Clinical rheumatology, 35(2),101692 (2021).
- Tiwari, V. & Brent, L.H. Psoriatic Arthritis. In StatPearls [Internet]. (StatPearls Publishing, 2022). https://www.ncbi. nlm.nih.gov/books/NBK547710/
- Cassell, S. & Kavanaugh, A. Psoriatic arthritis: pathogenesis and novel immunomodulatory approaches to treatment. Journal of immune based therapies and vaccines, 3, 6 (2005).
- Menter, A. Psoriasis and psoriatic arthritis overview. The American journal of managed care, 22(8 Suppl), s216–s224 (2016).
- Kirkham, B., et al. Early treatment of psoriatic arthritis is associated with improved patient-reported outcomes: finding from the etanercept PRESTA trial. Clinical and experimental rheumatology, 33(1), 11–19 (2015).
- Clark, B.M. Rheumatology: 9. Physical and occupational therapy in the management of arthritis. Canadian Medical Association journal, 163(8), 999–1005 (2000).
- Di Minno, M.N., et al. Weight loss and achievement of minimal disease activity in patients with psoriatic arthritis starting treatment with tumour necrosis factor α blockers. Annals of the rheumatic diseases, 73(6), 1157–1162 (2014).
- Letter on behalf of EC Europe - 9 Feb 2022.
April 3, 2023
Content Disclaimer:
You understand and acknowledge that all users of the Dis-Chem website or app are responsible for their own medical care, treatment, and oversight. All of the content provided on the website, are for INFORMATIONAL PURPOSES ONLY and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. The content is not intended to establish a standard of care to be followed by a user of the website. You understand and acknowledge that you should always seek the advice of your physician or other qualified health provider with any questions or concerns you may have regarding your health. You also understand and acknowledge that you should never disregard or delay seeking medical advice relating to treatment or standard of care because of information contained in or transmitted through the website. Medical information changes constantly. Therefore the information on this website or on the linked websites should not be considered current, complete or exhaustive, nor should you rely on such information to recommend a course of treatment for you or any other individual. Reliance on any information provided on this website or any linked websites is solely at your own risk.





