Autoimmune Diseases
Autoimmune Diseases


Back to top
CONTENTS
Back to top
WHAT IS AUTOIMMUNE DISEASE?
A healthy immune system defends the body against infectious agents and disease.1,4In people with autoimmune disease, the immune system cannot distinguish ‘self from non-self’ and as a result attacks its own healthy cells, tissue and organs.2,3,4,7,9
There are more than a 100 AUTOIMMUNE DISEASES recognised globally !1,2,7,9
Back to top
HOW DOES AUTOIMMUNE DISEASE DEVELOP?
The exact cause of autoimmune disease is not known but there are certain known factors that contribute to the development of some common disorders. Genetic characteristics (race, gender, ethnicity), environmental factors, certain viruses or bacteria can in some ways be linked to the development of an autoimmune disease as well as overuse of antibiotics.1,2,4,5,7
Back to top
GENETIC PREDISPOSITION (RACE, GENDER & AGE)
Gender Did you know that autoimmune disease affects women more than men? More than 75 % of people affected by autoimmune disease are female.3,9 Genetics There is a strong link between genetics and autoimmune disease. If an autoimmune disease occurs in the family history, then it predisposes an individual in future generations to developing one.3,9 Race Race also plays a role in the prevalence of autoimmune disease. Lupus and systemic sclerosis are more common in African Americans compared to Europeans, also experiencing disease earlier in life and to a more severe extent. However, the same populations also have a lower risk for type 1 diabetes, multiple sclerosis and thyroiditis.9 There are currently no genetic tools to predict the risk of developing an autoimmune disease
Back to top
ENVIRONMENTAL FACTORS
There is increased evidence suggesting that autoimmune disease development results from interaction with certain environmental factors.1,4 These factors may include:
- Harmful pathogens (viruses or bacteria)4
- A disrupted natural microbiome – especially in the gut, lungs or skin, often caused by the overuse of antibiotics4
- Nutrition like vitamin D, iodine and gluten4
- Tobacco smoke or exposure to heavy metals.4,5 Smoking has specifically been identified as a risk factor for developing rheumatoid arthritis & lupus.4

Back to top
HOW ARE AUTOIMMUNE DISEASES DIAGNOSED?
The diagnosis of autoimmune disorders presents a challenge to both doctors and patients. Early signs and symptoms can be non-specific, adding to the possibility of a variety of illnesses.6 Symptoms may also be intermittent, and present in different ways in different individuals. This leads to a complicated diagnostic process that can place a stressful and a psychological burden on patients.5,6,7,9 A thorough family disease history is needed followed by a proper physical examination.6 If an autoimmune disease is suspected, further diagnostic blood tests will be performed.4,6,7 Imaging tests, like magnetic resonance imaging (MRI) (detailed images of organs, tissue and bones) and ultrasound (creates pictures of internal structures), may also be conducted to rule out any infections, fractures or tumours that may cause similar symptoms to those of autoimmune disease.6
Back to top
HOW COMMON ARE AUTOIMMUNE DISEASES?
In general, autoimmunity affects 5 – 9 % of the population. Collectively, autoimmune diseases are considered common with an increasing incidence, the reason for which is unclear.1,4,9
Back to top
COMMON AUTOIMMUNE DISEASES
Body cells use glucose to produce energy for normal bodily functions. The body’s reaction to sugar (glucose) we ingest through food, is to produce insulin, a hormone produced by beta cells in the pancreas.10 In patients suffering from Type 1 Diabetes Mellitus, the body produces antibodies that attack and destroy these pancreatic beta cells – the result being that they are unable to produce any insulin.10 Before diagnosis, these patients usually suffer from excessive thirst, frequent urination, weight loss, high blood glucose levels and delayed growth in infants.10 Type 1 diabetes can be managed by insulin injections diet, exercise and close monitoring of blood glucose levels. Frequent screenings for diabetic complications (high blood pressure, high cholesterol, visual loss and neuropathy) must be carried out.10
Back to top
MULTIPLE SCLEROSIS (MS)
Back to topMULTIPLE SCLEROSIS (MS)
Multiple sclerosis is a chronic inflammatory disorder of supposed autoimmune etiology, that can be divided into three broad disease stages:11
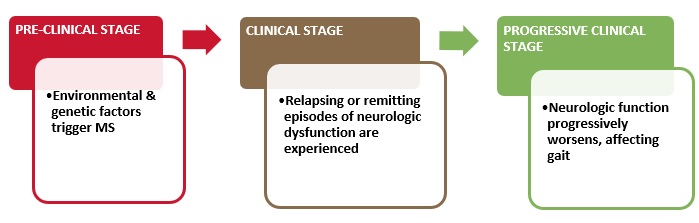
Due to good progress made in understanding the complexity of MS, treatments for the relapsing and inflammatory stage of the disease are readily available.11
Back to top
IRRITABLE BOWEL SYNDROME (IBS)
Irritable Bowel Syndrome (IBS) is an umbrella term for both abdominal discomfort (or pain) with disrupted defecation (as either diarrhoea or constipation).12
Patients suffering from IBS can suffer from predominant constipation or diarrhoea or a combination of both.12 IBS is considered to be one of the most common ADs and straightforward to diagnose.12 Treatment does not target the underlying cause but rather focuses on the symptoms.12 Fibre supplements and adequate fluid intake can be effective for those with constipation and can help firm up stools in patients with predominant diarrhoea.12 Antispasmodic agents are helpful for abdominal pain or cramps and antidiarrheals such as loperamide are of value in patients with predominant diarrhoea.12 Prescribed medications can be used for patients with resistant symptoms.12 The link between IBS and INTESTINAL MICROBIOME Alteration in the gut microbiome (flora) is accepted as a cause for IBS. Subsequently, changes in gut flora are linked to low-grade INFLAMMATION. An overgrowth of bacteria in the small intestines is also present in some patients presenting with IBS symptoms.16 A general consensus under healthcare professionals is the addition of probiotics supplements for patients suffering from IBS as studies found that probiotics decreases IBS symptoms globally and provide promising results by maintaining gut BALANCE.12,16 Systemic Lupus Erythematosus Systemic Lupus Erythematosus (called Lupus for short) is a chronic, inflammatory autoimmune disease that affects multiple organs and up to 5 million people globally. In patients with Lupus, the immune system produces antibodies that attack healthy tissue in organs throughout the body resulting in a variety of clinical conditions. Lupus is 10 x more likely in women compared to men. Lupus can lead to the development of atherosclerosis, infections, cancer and organ damage, especially end-stage kidney disease.13 Treatment is directed to the patient’s specific organ system involvement.13 Drugs used in the treatment of Lupus include anti-inflammatories, corticosteroids and other immunosuppressants.4,13
Back to top
RHEUMATOID ARTHRITIS (RA)
Rheumatoid Arthritis is an autoimmune disease that affects the joints. This disease mostly affects the same joints on both sides of the body (for example the hands, wrists, knees, jaw and feet). Immune cells attack the body’s joint tissue, resulting in swelling, inflammation, joint stiffness and pain.14 Symptoms and risk factors Patients with undiagnosed RA may experience occasional low-grade fever, a loss of appetite and feel unusually tired. Joint stiffness (for more than 30 minutes) and joint pain (during movement and rest) are also an indication of RA.14 Symptom flare-ups may be caused by stress, excessive physical activity and the sudden withdrawal of certain medications.14 People that are at risk include:14
- The elderly
- Female gender
- Family history
- Obesity
- Tobacco smoke
- Gum disease
Back to top
GRAVES’ DISEASE
Graves’ disease is an autoimmune disease that develops when the body’s immune system produces specific antibodies that attach onto the thyroid cells and stimulate excessive thyroid hormone production.15 The thyroid is a butterfly-shaped organ located on both sides of the trachea in the neck.15 Excessive thyroid hormone production leads to hyperthyroidism.15 This in effect can cause irregular heart rhythm that can lead to blood clots, stroke or heart failure in the long term, and decreased bone-density and osteoporosis.15 Other symptoms include:
- Diarrhoea (frequent bowel movements) and weight loss15
- Heat intolerance, nervousness and irritability15
- Tremors (hands)15
- Trouble sleeping15
- Tired or weakened muscles15
- Abnormal enlargement of the thyroid gland15
- Treatment can include medication, radioiodine therapy or thyroid surgery.15
Back to top
FUTURE DEVELOPMENTS
Treatments for autoimmune diseases are constantly under review and drastic progress has been made in developing new therapies as more is discovered about complex autoimmune diseases. The relationship between a disrupted gut microbiome and autoimmune diseases is increasingly prevalent. Probiotics are ‘live microorganisms that have been considered to enhance health when administered in adequate amounts to the host’.16 They are used in various conditions for their functions in restoring gut flora BALANCE and maintaining a healthy intestinal (gut) barrier. Disruption of the barrier function in the gut is linked abnormal immune responses. Probiotics also have a role to play in stimulating or suppressing immunity, regulating appropriate immune responses and resulting inflammation. Future treatments could include the possibility of restoring the gut microbiome to regulate inflammatory processes in autoimmune diseases.16,17
Last reviewed : 5 May 2024
Back to top
DEAL WITH AUTO IMMUNE DISEASE BY ALWAYS STARTING WITH YOUR GUT
Autoimmune disease is when the immune system reacts to its own tissues and cells as if they are foreign invaders by attacking them by mistake leading to chronic inflammation.1 Trillions of bacteria living in your gut make up your gut microbiota, where they aid digestion, prevent infection, produce certain vitamins, educate (signal) and support our immune system and help protect us from autoimmune diseases.2 The immune system needs to be in balance and stay strong and alert to protect the body against foreign invaders that cause illness, but at the same time need to recognize the body’s own tissues and organs and protect them from being attacked.Research shows that there is a connection between the gut microbiome and the immune system and if there are dysfunctions in both these systems, they can contribute to autoimmunity resulting in rheumatoid arthritis, lupus, multiple sclerosis, diabetes, Grave’s disease and inflammatory bowel disease.3 There are also other issues that disrupt the delicate balance of the gut microbiome, such as stress, illness, poor diet and use of antibiotics.4 These all affect the intestinal barrier, upset digestion and cause widespread inflammation throughout the body.5,6,7 Medical (Clinical) researchers are now realizing the benefits of using probiotics to manage autoimmune diseases.1,2 Probiotics can improve the function of the intestinal barrier, protect it from damage and prevent pathogens from passing into the bloodstream and igniting the autoimmune response.3,4,5,6
Spore-based probiotics stimulate the production of key immune cells that protect us against pathogens, as well as reducing the incidence to allergy and infection, small intestinal bacterial overgrowth, abdominal pain, bloating and diarrhoea.1 As these spore-based probiotics do not contain any live bacillus strains, only its spores, they are unaffected by antibiotics and survive stomach acid making sure that healing quantities reach the lower intestine where they are needed most.2,3 It is here in the small intestine where sporebiotics reduce inflammation, prevent toxins being released into the blood stream, facilitate the proper digestion of food and support the immune system, reducing the likelihood of autoimmune disease.4
Medical References

October 5, 2021
Content Disclaimer:
You understand and acknowledge that all users of the Dis-Chem website or app are responsible for their own medical care, treatment, and oversight. All of the content provided on the website, are for INFORMATIONAL PURPOSES ONLY and DOES NOT CONSTITUTE THE PROVIDING OF MEDICAL ADVICE and is not intended to be a substitute for independent professional medical judgment, advice, diagnosis, or treatment. The content is not intended to establish a standard of care to be followed by a user of the website. You understand and acknowledge that you should always seek the advice of your physician or other qualified health provider with any questions or concerns you may have regarding your health. You also understand and acknowledge that you should never disregard or delay seeking medical advice relating to treatment or standard of care because of information contained in or transmitted through the website. Medical information changes constantly. Therefore the information on this website or on the linked websites should not be considered current, complete or exhaustive, nor should you rely on such information to recommend a course of treatment for you or any other individual. Reliance on any information provided on this website or any linked websites is solely at your own risk.